Throughout the centuries, there have been many theories for what causes migraines. While the exact cause of migraines is still not fully understood, a combination of genetic, environmental, and neurological factors likely contribute to their development. Understanding these factors can help individuals better manage and prevent migraine episodes.
A migraine is a neurological condition that causes recurring episodes of severe headaches that can be debilitating for those who experience them. Here is a breakdown of some known factors that can make somebody more likely to experience migraines.
The most common contributing factors for migraine
- Genetics: Studies have shown that migraine tends to run in families, suggesting that there may be a genetic component to the condition. Researchers have identified several genetic subtypes that appear to be associated with an increased risk of developing migraine. However, it’s worth noting that having these genes doesn’t necessarily mean that a person will develop migraines, as other factors can also play a role. The only form of migraine with a definite genetic predisposition is a familial hemiplegic migraine.
- Hormones: Hormonal changes are a common trigger for migraines in women, and many women report that their migraines are linked to their menstrual cycle. This suggests that fluctuating estrogen levels and other hormones may play a role in migraine development. As estrogen levels fall during the menstrual cycle, so does serotonin, which increases the overall sensitivity of the brainstem and makes a migraine more likely. Additionally, some women experience a reduction in migraines after menopause, further supporting the idea that hormones may be involved.
- Environmental factors: Various environmental factors have been linked to an increased risk of migraine, including changes in weather patterns, exposure to bright lights or loud noises, and certain smells or chemicals. Stress is also a well-known trigger for migraine, and many people report that their migraine episodes occur during or after periods of high stress.
- Lifestyle factors: Certain lifestyle factors have been associated with an increased risk of migraine. For example, people who don’t get enough sleep or have irregular sleep patterns are more likely to experience migraine episodes. Fasting or skipping meals will reduce blood glucose levels, which is also known to be a contributing factor for migraines. Additionally, certain foods or drinks, such as alcohol, caffeine, or processed meats, may trigger migraine in some people. Physical activity can either trigger or relieve migraine, depending on the individual.
- Neurological factors: Migraine is a neurological condition, so it makes sense that some neurological factors would be involved in its development. Researchers have found that people with migraines tend to have differences in how their brain processes sensory information and specific areas of the brain may be more sensitive to certain triggers. Disruption to regular sleep and stress are two factors that can affect these brain regions.
- Musculoskeletal factors: The nerves from structures in the upper neck (muscles, joint capsules, ligaments etc.) converge on the brain area responsible for the headache component of migraine. Prolonged stress on these structures can make this area of the brain more sensitive and, therefore, more susceptible to migraine.


Overall, it’s likely that migraine episodes are caused by a combination of these factors rather than any single cause. Additionally, each person’s experience with migraine is unique, and what triggers one person’s migraine may not be the same as what triggers someone else’s. As a result, treatment for migraine must be individualised and may involve a combination of lifestyle changes, medications, and other interventions.
Common treatments for migraine
Some of the most common treatments for migraines include:
- Lifestyle changes: Adjusting your diet, sleep habits, and stress levels can help reduce the frequency and severity of migraine. This might involve avoiding certain trigger foods, establishing a regular sleep routine, or practising relaxation techniques like yoga or meditation.
- Medications: Several medications may be used to treat migraines, including pain relievers, triptans, and preventative medications. Pain relievers like aspirin or ibuprofen can help to relieve the symptoms of a migraine. At the same time, triptans can reduce the nervous system’s sensitivity if taken early during a migraine episode. Preventative medications, such as antidepressants or CGRP therapies, may be used to reduce the frequency or severity of migraine. It is essential to consult with your doctor or neurologist to ensure that these medications are proper for you and will not cause adverse effects.
Various non-pharmacological treatments for migraine have been tested scientifically for their effectiveness.
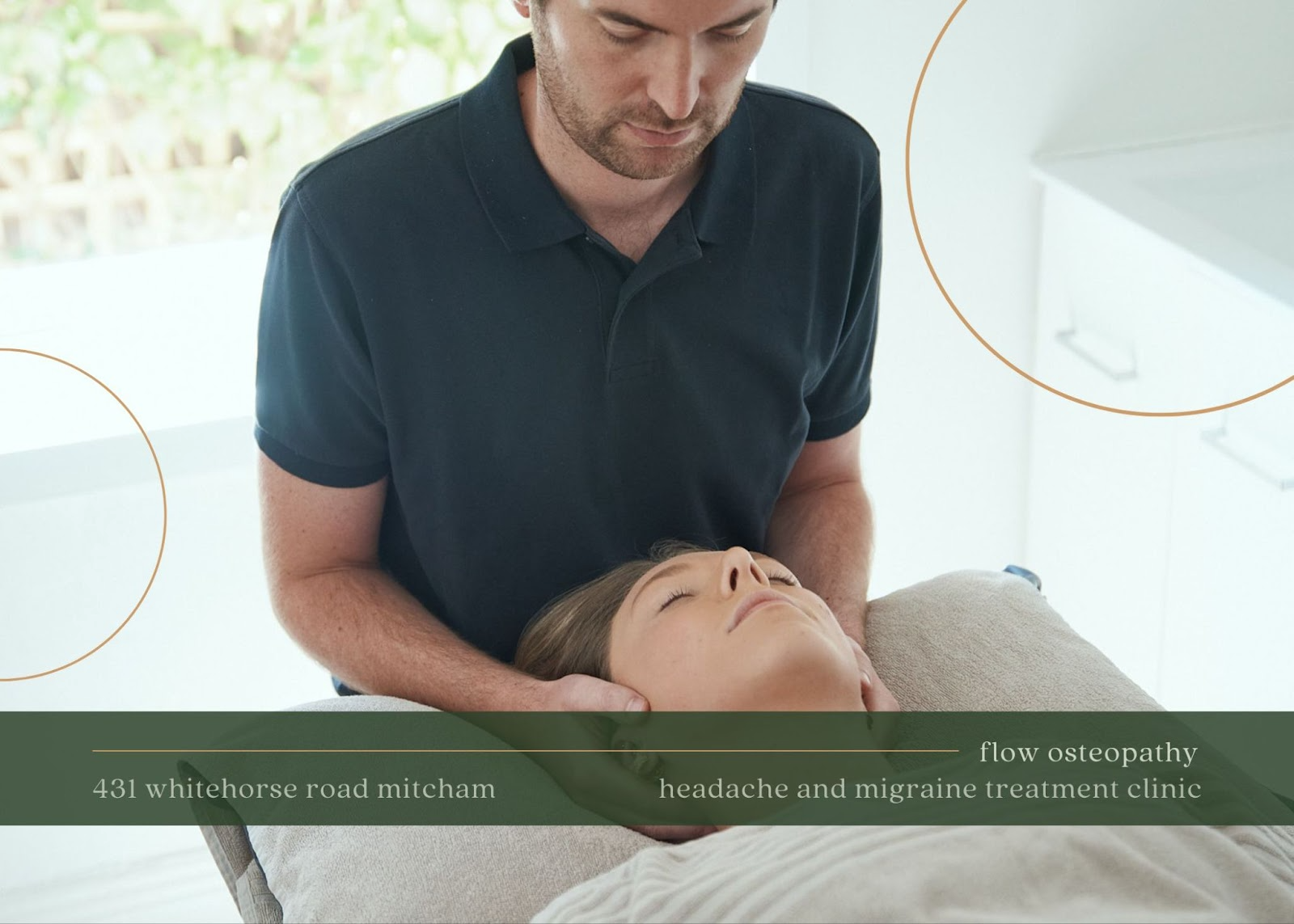
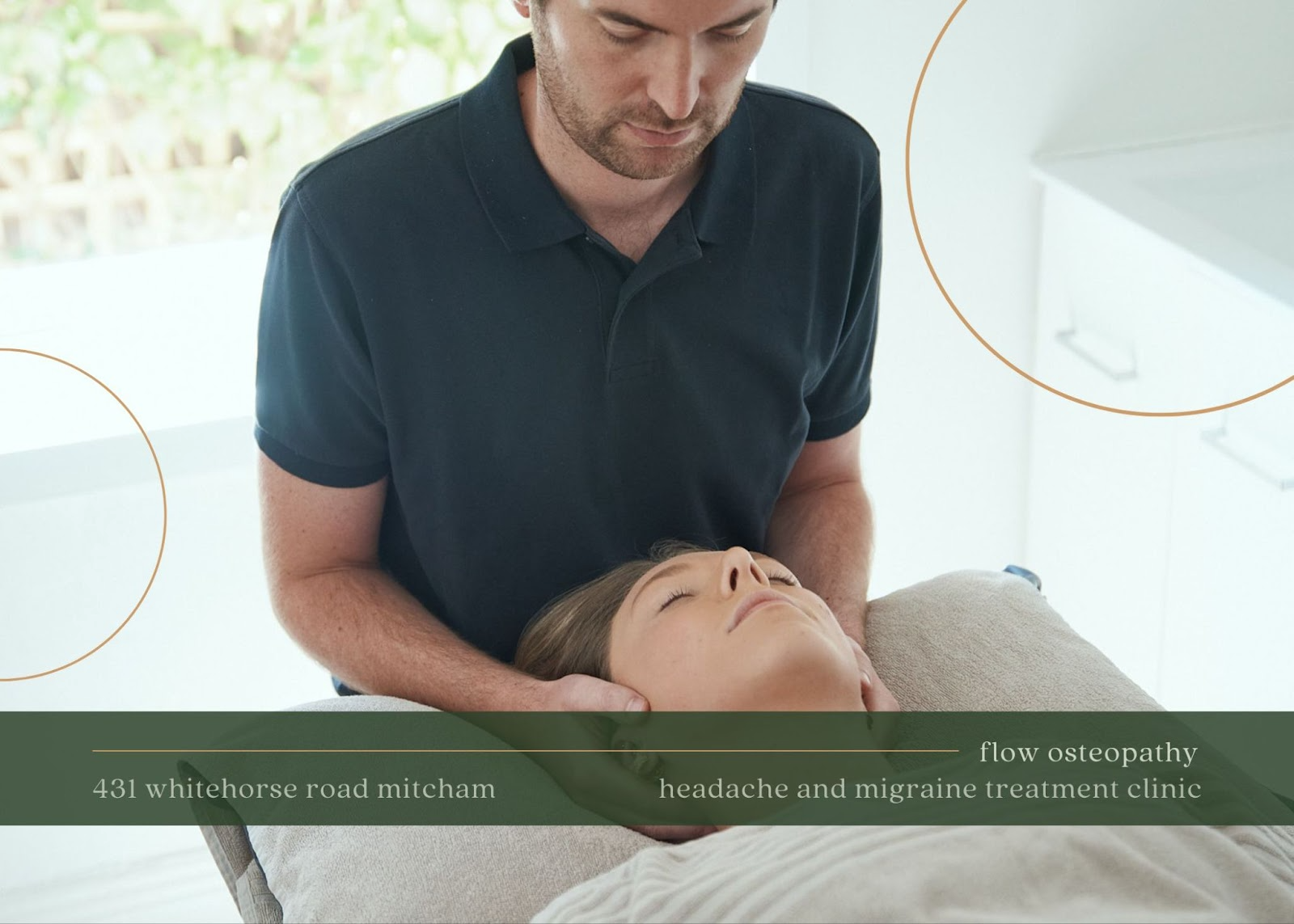
At Flow Osteopathy, our treatment plan is based on the Watson Headache Approach, an evidence-based treatment for migraine and headaches. It focuses on resolving issues with the upper neck, which is one of the contributing factors for migraine.
Final thoughts on migraine
Migraine can be a debilitating and confusing condition, and its causes are complex. Various factors, including lifestyle, neurological, and musculoskeletal problems, can be associated with migraine. There is no one specific cause.
Fortunately, various treatments are available for managing migraine symptoms, including lifestyle modifications, medications, and the Watson Headache Approach.
It is vital to work with your osteopath to find the best treatment plan that works for you and your lifestyle.Book an appointment with one of our experienced practitioners at Flow Osteopathy for a comprehensive assessment and treatment plan.